Where it all started!
Our self-absorption with physical appearance takes us back to Eve (first woman). Do you know what actually appealed to Eve about the forbidden fruit?

“When the woman saw that the fruit of the tree was good for food and pleasing to the eye, and also desirable for gaining wisdom, she took some and ate it.” Genesis 3: 6, italics further added that the fruit had a functional appeal; it also appealed to her desire for enhancing insight and perception. But equally important was the fact that it was “pleasing to the eye” i.e. it was physically attractive. This preferance that Eve bestowed on physical beauty thus became the accepted pattern for all human beings.
This deception that physical attractiveness is to be held above the beauty of heart and life, leaves both the genders especially women, feeling unattractive, ashamed, and hopelessly flawed.
What is Body Dysmorphic Disorder?
So this overzealous drive of some individuals to always look breath-taking, may develop into a psychiatric condition which is recognized as body dysmorphic disorder.

Body dysmorphic disorder (BDD) was discovered in 1891 and was then called
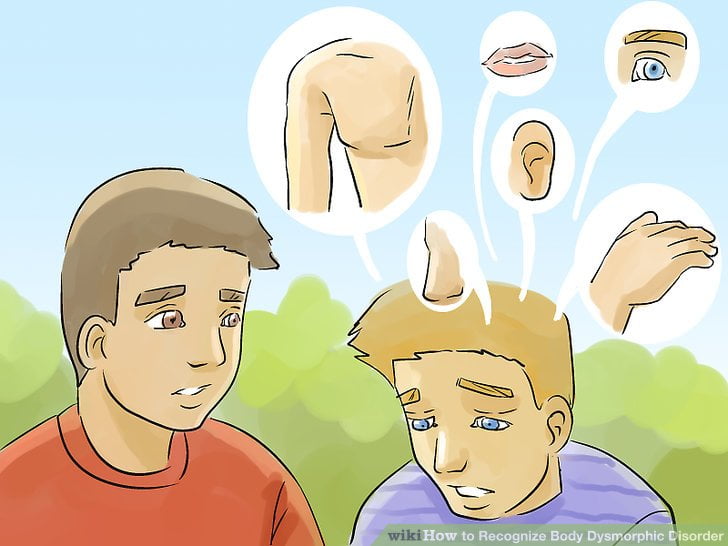
Some of the most common body parts that one fixates on are
- Moles and freckles
- Scars or aberrations
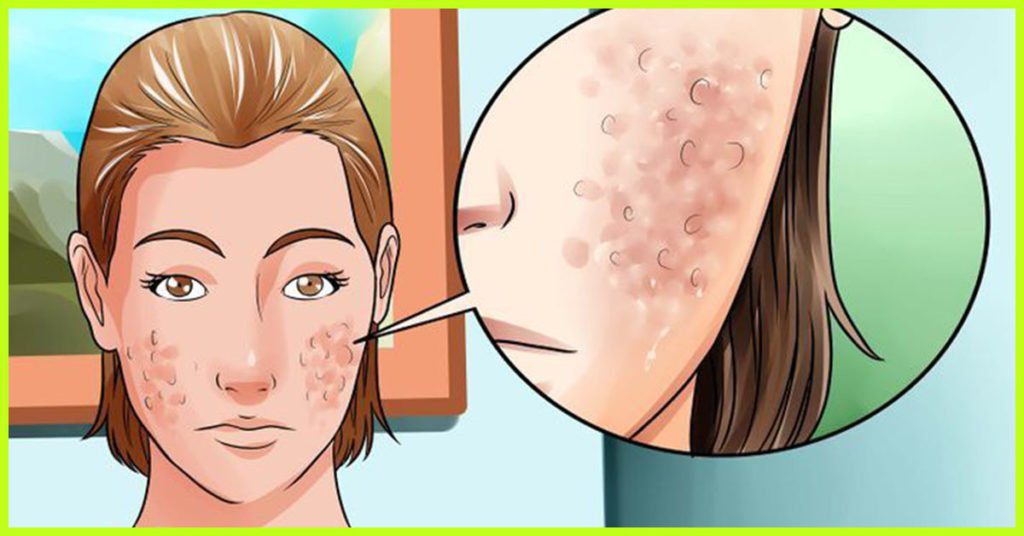
- Acne
- Facial and body hair
- Balding or hair thinning
- Size and shape of genitalia and breasts
- Muscle size (also known as muscular dysmorphia)

muscle dysmorphia 

acne 
moles
Still, this list is not exhaustive and a perceived flaw can be present anywhere on the body.
Identifying Body Dysmorphic Disorder
Body dysmorphic disorder is similar to both obsessive-compulsive disorder and eating
Causes and Risk Factors
Exact causes of BDD are still unknown. However, according to recent studies there are different risk factors:
- Childhood adversity, such as abuse or bullying
- low self-esteem
- fear of being isolated
- perfectionism, shyness
- depression, anxiety and OCD
- A genetic predisposition.
- A history of dermatological or other physical stigmata as an adolescent, since resolved.
- Being aesthetically sensitive than average.


Bullying
Symptoms
- Being grossly preoccupied with a hypothetical flaw in appearance that to others appears minor.
- Belief that you have a fault in your looks that makes you unattractive or deformed.
- Belief that people mock you for your appearance.
- Engaging in behaviours aimed at fixing the perceived flaw, such as frequently checking the mirror, skin picking, styling, makeup or wearing something suitable.
- Constant comparisons with peers or celebrities.
- Seeking cosmetic procedures.
- Avoiding social interactions
- Being so obsessed with appearance that it leads to major distress in your social life, work, or other areas of functioning
- Seeking constant reassurance about how you look.
- Excessive exercising
- Changing clothes frequently.

Cosmetic surgery 
Ironically, the pursuit of physical beauty is an unattainable goal—always out of reach.
Diagnosis
Unfortunately, most of the times body dysmorphic disorder may go undiagnosed. This happens since most of the individuals with BDD are discreet about their obsessions and compulsions. Many times, it is misdiagnosed as social phobia or a depressive disorder. One important clue though is repetitive cosmetic surgeries for the same or multiple perceived physical flaws. Once suspected for BDD, patient is likely to be sent to a mental health professional who will further complete assessment taking in consideration patient’s attitude, behaviours, signs and symptoms.
The two common treatment options for body dysmorphic disorder is Medication and Cognitive behavioral therapy.
Cognitive behavioral therapy:
Cognitive behavioral therapy is a coping technique that teaches the patients, how to recognize irrational thoughts and cut down the negative thinking and practice positive thinking. Exposure and response prevention are two important techniques involved. Exposure helps to confront situations that causes irrational fear (e.g., going out in public with the perceived flaw without appropriate clothing). Response prevention helps in overcoming the urge to cover up the perceived flaw with makeup or clothing, seeking reassurance from peers about your appearance, and decrease the amount of time spent on repeatedly checking yourself in front of the mirror.
Medications :

Antidepressants, specifically, Selective Serotonin Reuptake Inhibitors (SSRIs) are prescribed. These are effective, because it is believed that a secondary cause of body dysmorphia is due to abnormalities in concentration of the brain chemical serotonin. In some situations, an anti-psychotic drug in addition to an antidepressant, is also prescribed especially if the patient complains of delusions.